WHAT IS MAMMOGRAPHY?
Mammography is a specific type of imaging that uses a low-dose x-ray system for examination of the breasts. Most medical experts agree that successful treatment of breast cancer often is linked to early diagnosis. Mammography plays a central part in early detection of breast cancers because it can show changes in the breast up to two years before a patient or physician can feel them.
Screening is key to the early detection of breast cancer. Annual screening mammography is currently recommended by most National organizations for all women over the age of 40. It can detect a cancer in the breast up to two years before a patient or physician can feel the lump. The Annex Medical Imaging is also a screening centre for the Ontario Breast Screening Program and has been accredited by the Canadian Association of Radiologists since 1998.
We have digital mammogram machine with low dose radiation and low compression.
It’s the Stenograph Pristina with Self Compression, also called the Stenograph Pristina Dueta, made by GE Healthcare.
It is the first mammography system with a patient assisted compression device, which is a wireless, handheld remote control that is used to adjust the compression after the breast has been positioned. The technologist then checks the compression to see if it is enough.
Self-compression “may be an effective mammography technique for women who want to take an active role in their own breast examination,” the researchers write. And their discomfort may go down.
Also, mammography exams are often scheduled at the early to middle stage of your menstrual cycle, when the breasts are less sensitive and easiest to image.
Following screening mammography, about 10% of women will be recalled for additional views. This should not cause undue worry as more than 9 out of 10 patients that get recalled for additional views are subsequently categorized as “benign” or “probably benign”.
If we feel that additional views are necessary, one of our staff will contact and schedule an appointment.
WHAT ARE SOME COMMON USES OF THE PROCEDURE?
Mammography is used to aid in the diagnosis of breast diseases in women. Screening mammography can assist your physician in the detection of disease even if you have no complaints or symptoms.
Initial mammography images themselves are not always enough to determine the existence of a benign or malignant disease with certainty. If a finding or spot seems suspicious, your radiologist may recommend further diagnostic studies.
Diagnostic mammography is used to evaluate a patient with abnormal clinical findings, such as a breast lump or lumps, that have been found by the woman or her doctor. Diagnostic mammography may also be done after an abnormal screening mammography in order to determine the cause of the area of concern on the screening exam.
HOW SHOULD I PREPARE FOR A MAMMOGRAM?
Before scheduling a mammogram it is recommended that you discuss any new findings or problems in your breasts with your doctor. In addition, inform your doctor of any prior surgeries, hormone use, and family or personal history of breast cancer.
Do not schedule your mammogram for the week before your period if your breasts are usually tender during this time. The best time to schedule is one week after your period. Always inform your doctor, radiologist, and x-ray technologist if there is any possibility that you are pregnant.
- Do not wear deodorant, talcum powder, or lotion under your arms or on your breasts on the day of the exam. These can appear on the x-ray film as calcium spots.
- Describe any breast symptoms or problems to the technologist performing the exam.
- If possible, obtain prior mammograms and make them available to the radiologist at the time of the current exam.
- Ask when your results will be available; do not assume the results are normal if you do not hear from your doctor.
- In addition, before the examination, you will be asked to remove all jewellery and clothing above the waist and you will be given a gown or loose-fitting material that opens in the front.
HOW DOES THE PROCEDURE WORK?
The breast is exposed to a small dose of radiation to produce an image of internal breast tissue. The image of the breast is produced as a result of some of the x-rays being absorbed (attenuation) while others pass through the breast to expose either a film (conventional mammography) or digital image receptor (digital mammography).
WHAT WILL I EXPERIENCE DURING THE PROCEDURE?
You will feel pressure on the breast as it is squeezed by the compressor. Some women with sensitive breasts may experience discomfort. If this is the case, schedule the procedure when your breasts are least tender. The technologist will apply compression in gradations. Be sure to inform the technologist if pain occurs as compression is increased. If discomfort is significant, less compression will be used.
WHAT ARE THE BENEFITS VS. RISKS?
Benefits
- Imaging of the breast improves a physician’s ability to detect small tumors. When cancers are small, the woman has more treatment options, and a cure is more likely.
- The use of screening mammography increases the detection of small abnormal tissue growths confined to the milk ducts in the breast, called ductal carcinoma in situ (DCIS). These early tumors cannot harm patients if they are removed at this stage and mammography is the only proven method to reliably detect these tumors.
Risks
- The effective radiation dose from a mammogram is about 0.7 mSv, which is about the same as the average person receives from background radiation in three months.
- Women should always inform their doctor or x-ray technologist if there is any possibility that they are pregnant.
- False Positive Mammograms. Five to 10 percent of screening mammogram results are abnormal and require more testing (more mammograms, fine needle aspiration, ultrasound or biopsy), and most of the follow-up tests confirm that no cancer was present. It is estimated that a woman who has yearly mammograms between ages 40 and 49 would have about a 30 percent chance of having a false-positive mammogram at some point in that decade, and about a 7 to 8 percent chance of having a breast biopsy within the 10-year period. The estimate for false-positive mammograms is about 25 percent for women ages 50 or older.
WHAT DOES THE MAMMOGRAPHY EQUIPMENT LOOK LIKE?
A mammography unit is a rectangular box that houses the tube in which x-rays are produced. The unit is dedicated equipment because it is used exclusively for x-ray exam of the breast with special accessories that allow only the breast to be exposed to the x-rays. Attached to the unit is a device that holds and compresses the breast and positions it so images can be obtained at different angles.
HOW IS THE PROCEDURE PERFORMED?
During mammography, a specially qualified radiology technologist will position you to image your breast. The breast is first placed on a special platform and compressed with a paddle (often made of clear Plexiglas or other plastic).
Breast compression is necessary in order to:
- Even out the breast thickness so that all of the tissue can be visualized;
- Spread out the tissue so that small abnormalities won’t be obscured by overlying breast tissue;
- Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged;
- Hold the breast still in order to eliminate blurring of the image caused by motion;
- Reduce x-ray scatter to increase sharpness of picture.
The technologist will go behind a glass shield while making the x-ray exposure, which will send a beam of x-rays through the breast to the film behind the plate, thus exposing the film.
You will be asked to change positions slightly between images. The routine views are a top-to-bottom view and a side view. The process is repeated for the other breast.
The examination process should take about half an hour. When the mammography is completed you will be asked to wait until the technologist examines the images to determine if more are needed.
WHO INTERPRETS THE RESULTS AND HOW DO I GET THEM?
A radiologist (a physician experienced in mammography and other x-ray examinations) will analyze the images, describe any abnormalities, and suggest a likely diagnosis. The report will be dictated by the radiologist, and then sent to your referring physician who will inform you of your test results.
Also Read: Pediatric abdominal ultrasound and preparation
WHAT ARE THE LIMITATIONS OF MAMMOGRAPHY?
Interpretations of mammograms can be difficult because a normal breast can appear differently for each woman. Also, the appearance of an image may be compromised if there is powder or salve on the breasts or if you have undergone breast surgery. Because some breast cancers are hard to visualize, a radiologist may want to compare the image to views from previous examinations. Not all cancers of the breast can be seen on mammography.
Breast implants can also impede accurate mammogram readings because both silicone and saline implants are not transparent on x-rays and can block a clear view of the tissues behind them, especially if the implant has been placed in front of, rather than beneath, the chest muscles. Patients with breast implants should inform the technologist.
Source: Canadian Association of Radiologists Patient Information
Preparation
MAMMOGRAPHY
Mammography is a specific type of imaging that uses a low-dose x-ray system for examination of the breasts. Most medical experts agree that successful treatment of breast cancer often is linked to early diagnosis. Mammography plays a central part in early detection of breast cancers because it can show changes in the breast up to two years before a patient or physician can feel them.
MAMMOGRAM PREPARATION
These instructions are IMPORTANT. Please follow them.
- If possible, obtain prior mammograms and make them available to the radiologist at the time of the current exam.
- Before scheduling a mammogram it is recommended that you discuss any new findings or problems in your breasts with your doctor. In addition, inform your doctor of any prior surgeries, hormone use, and family or personal history of breast cancer.
- Do not schedule your mammogram for the week before your period if your breasts are usually tender during this time. The best time to schedule is one week after your period. Always inform your doctor, radiologist, and x-ray technologist if there is any possibility that you are pregnant.
- Do not wear deodorant, talcum powder, or lotion under your arms or on your breasts on the day of the exam. These can appear on the x-ray film as “calcium”.
- Describe any breast symptoms or problems to the technologist performing the exam.
- Ask when your results will be available; do not assume the results are normal if you do not hear from your doctor.
In addition, before the examination, you will be asked to remove all jewelry and clothing above the waist and you will be given a gown or loose-fitting material that opens in the front.
continue reading
Related Posts
pelvic ultrasound is most often used to examine the uterus and ovaries and, during pregnancy, to monitor the health and development of the embryo or fetus
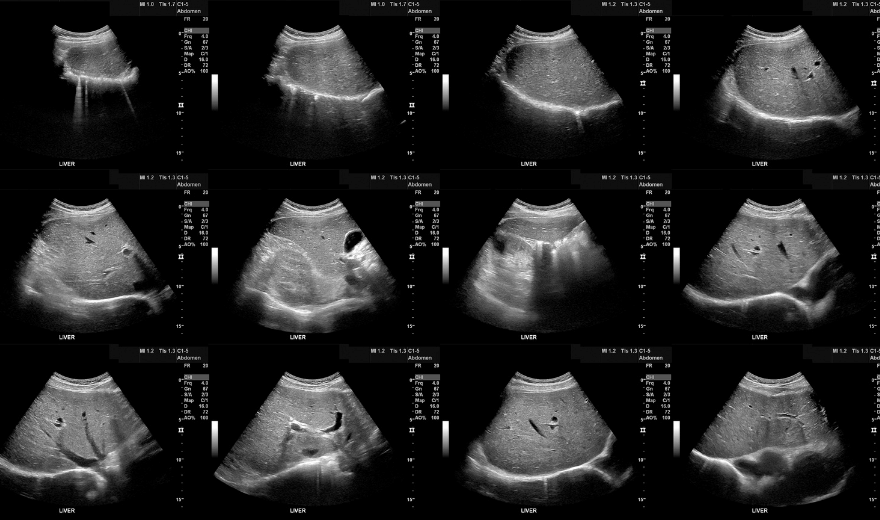
Ultrasound imaging, also called ultrasound scanning or sonography, involves exposing part of the body to high-frequency sound waves to produce pictures of the inside of the body.
An abdominal ultrasound image is a useful way of examining internal organs, including the liver, gallbladder, spleen, pancreas, kidneys, and bladder.